What Every Mom-to-be Should Know About Vaginal Prolapse
- Lifestyle
-
- UPDATED November 27, 2024
by Tasha Mayberry
995 shares

Vaginal prolapse is a condition in which one or more pelvic organs descend and press against or protrude through the vaginal canal. This often occurs when the pelvic floor muscles and connective tissues weaken or are damaged, leading to insufficient support for these organs.
While it can affect women of all ages, it is most common among those who have given birth or are postmenopausal. The American Journal of Obstetrics & Gynecology identifies vaginal childbirth as the leading modifiable risk factor for prolapse. It is strongly linked to pelvic floor disorders and stress incontinence.
Despite its prevalence, vaginal prolapse is often overlooked or misunderstood, leaving many women unaware of the symptoms, causes, and treatment options.
This article delves into the specifics of vaginal prolapse, aiming to shed light on its management and the importance of early intervention.
Types and Degrees of Vaginal Prolapse
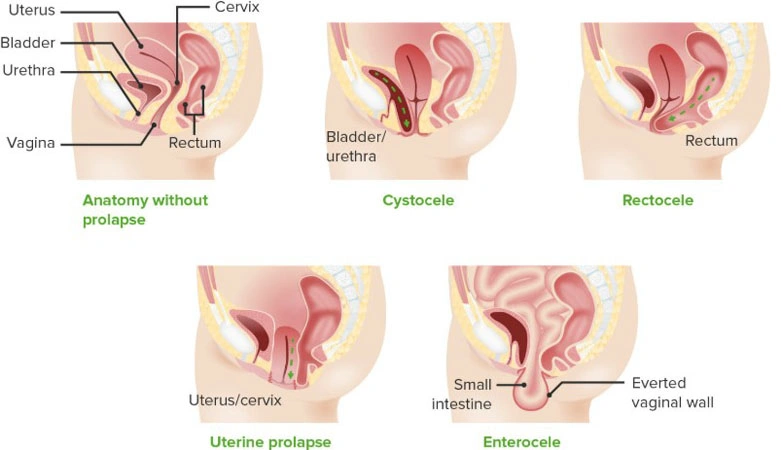
Your pelvis contains the vagina, uterus, rectum, bladder and urethra. Vaginal prolapse can take several forms, depending on which pelvic organ is involved.
According to the Cleveland Clinic, cystocele occurs when the bladder bulges into the vaginal wall, and rectocele involves the rectum pressing against the vagina. Uterine prolapse, on the other hand, is characterized by the uterus descending into or out of the vaginal canal. For women who have had a hysterectomy, vaginal vault prolapse may occur, where the top of the vaginal canal loses its support and falls.
The severity of prolapse is graded into stages, ranging from mild to severe. In Stage 1, the organ shifts only slightly downward but remains within the vagina. By Stage 4, the organ may completely protrude outside the vaginal opening, causing significant discomfort and impairment. Recognizing these stages is critical in determining the appropriate treatment approach.
Causes and Risk Factors
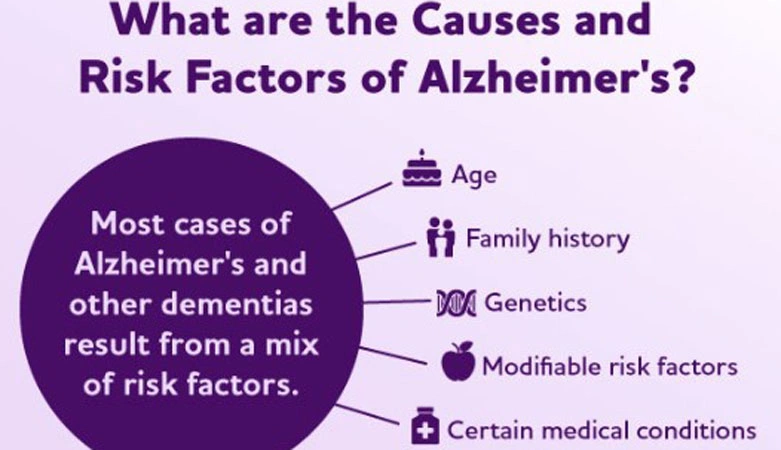
The underlying cause of vaginal prolapse lies in the weakening of the pelvic floor muscles and connective tissues.
Mayo Clinic writes that several factors contribute to this weakening, with childbirth being a primary cause. Vaginal deliveries, especially those involving larger babies or the use of forceps, can stretch and strain the pelvic structures. Aging and menopause further increase the risk, as the natural decline in estrogen levels leads to reduced muscle and tissue strength.
Chronic conditions that increase intra-abdominal pressure, such as persistent coughing, obesity, and constipation, are also significant contributors. Repeated straining over time can overstress the pelvic floor, exacerbating the likelihood of prolapse.
Additionally, some women are genetically predisposed to connective tissue weaknesses, making them more vulnerable.
Lifestyle factors, including heavy lifting or high-impact activities, can further heighten the risk. Preventing these contributing factors through education and early lifestyle adjustments can play a key role in mitigating the risk of prolapse.
Symptoms and Diagnosis
The symptoms of vaginal prolapse vary depending on the type and severity but commonly include a feeling of pressure or fullness around the vagina.
According to Johns Hopkins Medicine, many women describe a heavy sensation around their lower abdomen or genitals. It might also feel like something falling out of your vagina or sitting on a ball. Difficulty with urination, such as the bladder not emptying completely, or bowel movements is also a frequent concern.
Diagnosis typically starts with a thorough pelvic exam conducted by a doctor. During the exam, the doctor may ask the patient to bear down or cough to observe the extent of the prolapse. Imaging tests like an MRI or ultrasound may be recommended for more complex cases, allowing for detailed visualization of the pelvic organs and tissues.

Treatment Options and Management Strategies
Treating vaginal prolapse involves a range of options that depend on the severity of the condition and the patient’s preferences. Non-surgical approaches are often the treatment administered first. Pelvic exercises, such as Kegels, are highly effective in strengthening the muscles that support the organs in the region.
Lifestyle improvements, such as maintaining a healthy weight, avoiding weight lifting, and managing chronic constipation, can also reduce symptoms and prevent further progression.
Surgical options are considered when non-surgical treatments fail to provide sufficient relief. A vaginal mesh is often inserted via surgical methods to restore the proper positioning of the organs and improve support.
But this too can have its side effects like pain during sex, bleeding, and infection. Therefore, many women wonder what can be used instead of mesh for prolapse.
According to TruLaw, alternatives to mesh include native tissue repair, which uses the patient’s own tissues to provide support. A biological graft derived from human or animal tissue can also be an option. Gynecare pro-life and vaginal pessary are also options for you when preventive treatments are not possible anymore.
Coping with Vaginal Prolapse and Seeking Support
Living with vaginal prolapse can be challenging, not only physically but also emotionally. Many women feel embarrassed or isolated due to the condition, which can affect their quality of life. But you should know that around one in every three women experience vaginal prolapse in their life, Johns Hopkins Medicine reports.
Support networks often play a vital role in coping. Joining support groups allows women to share their experiences, get better informed, and build a sense of camaraderie. Emotional support from loved ones and clear communication with doctors are equally important in fostering confidence and resilience.
Routine follow-ups with a healthcare provider are vital in monitoring the condition and ensuring that management strategies remain effective. Empowering women with knowledge and resources can help them navigate the challenges of living with prolapse and improve their overall well-being.
FAQs
Can vaginal prolapse be prevented without surgery?
Yes, prevention is possible by strengthening pelvic floor muscles through exercises like Kegels, maintaining a healthy weight, and avoiding activities such as heavy lifting. Managing chronic conditions like constipation also helps reduce risk. Additionally, adopting good posture and using proper lifting techniques can further protect the pelvic floor and minimize strain.
How does vaginal mesh work?
The mesh is surgically implanted to reinforce the vaginal wall or support organs like the bladder, uterus, or rectum. It helps hold these organs in their proper position, restores pelvic stability, and reduces symptoms such as pressure, bulging, or incontinence.
What are the alternatives to surgical mesh for prolapse repair?
Alternatives include native tissue repair, which uses your own tissues, and biological grafts derived from human or animal tissue. These options avoid potential complications associated with synthetic mesh while providing effective and long-lasting results for many patients.
Overall, vaginal prolapse is a condition that no mother-to-be should feel embarrassed about. By understanding its causes, symptoms, and treatment options, you can take proactive steps to protect your pelvic health during and after pregnancy.
Breaking the silence around this common condition is crucial. If you notice any symptoms, be sure to consult a healthcare professional without delay. Addressing the issue early can greatly improve your comfort and confidence, allowing you to fully enjoy your journey into motherhood.